Cystocele is a pathology in which, due to weakening-stretching of the wall separating the bladder and vagina, the bladder invades the vagina. It is also called bladder hernia or bladder prolapse. At this time, due to the omission of the anterior wall of the vagina, the triangle and the neck of the bladder are displaced downward from their normal position.
This pathology is mainly observed in women over 40 years of age.
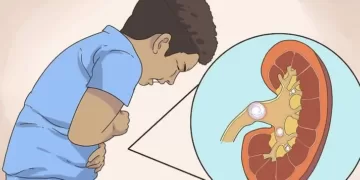
Its mechanism is associated with stretching-relaxation of the ligamentous apparatus of the pelvic diaphragm. This is due to hypotrophy of the muscular apparatus of the pelvic floor, as a result of which the anterior wall of the vagina protrudes. Along with the protrusion of the anterior wall of the vagina, there is insufficiency of the bladder and a shortening of the tube that removes urine. Such changes in the topography of the lower urinary tract cause symptoms of cystocele. Symptoms: difficulty urinating with residual urine, stress urinary incontinence up to complete urinary incontinence.
Causes and contributing factors of cystocele.
Among the main reasons for the development of cystocele, it is worth noting a birth injury with a rupture of the esophagus.
Among the predisposing factors, the professional activity of the patient associated with high physical activity is distinguished. Abdominal and pelvic floor pressure, excessive straining during childbirth, chronic constipation, heavy lifting, chronic cough, etc.
This pathology is mainly the destiny of the elderly and women who have given birth many times.
The pelvic floor is made up of a layer of muscles and tendons that hold the pelvic organs in the correct position.
Occupies the bladder, uterus, large and small intestines. If this supporting tissue base is weakened and stretched, then part of the pelvic organs will be displaced downward, and part will fall into a certain bulge.
Risk factors for developing a cystocele
- Childbirth – Pregnancy and childbirth are generally the most common causes of cystocele development. During childbirth, the muscles and tendons that hold the vagina are overstretched, which contributes to the weakening and stretching of the tissues that hold the organs in a normal position.
- Aging – The risk of developing a cystocele increases with age. Because the likelihood of stretching the pelvic diaphragm increases due to age-related weakening and gradual stretching of the muscular apparatus. Cystocele often occurs during menopause, when the body’s levels of estrogens (female sex hormones) decrease. Estrogens physiologically provide the tone of the muscular system.
- Hysterectomy – excision of the uterus often leads to weakening of the pelvic floor muscles.
- Genetic factors – a certain proportion of women are born with relatively weak connective tissue, which causes a predisposition to the development of cystocele. This is confirmed by the fact that not all women who have given birth many times or who have a lot of physical activity have the named pathology.
Adviсe:

- Don’t lift weights. Lift the load correctly – distribute the main load on the legs, and not on the back and hips.
- Pay attention to your diet. If you are prone to constipation, stay away from fiber-rich foods. Treat and prevent constipation!
- Do not smoke! Avoid prolonged coughing. Be sure to seek treatment if you experience this symptom or bronchitis.
- Control your weight. Gaining weight will make your condition worse.
When should you see a doctor?
A mild cystocele does not require medical attention.
In the case of moderate to severe form, when a person has the following symptoms, you should consult a doctor:
- Discomfort when urinating
- Urinary incontinence
- The feeling of heaviness in the vagina and pelvis
- Small bump at the entrance to the vagina
- Recurrent bladder infections
- Pain during intercourse requires a doctor’s consultation.
Treatment includes:
Therapeutic and preventive gymnastics to strengthen the pelvic floor
Estrogen therapy to increase muscle tone (tablets or special ointments topically).
The so-called Introduction of vaginal pessaries – a special plastic or rubber ring into the vagina to fix the bladder in the back and top position. For the same purpose, women are sometimes advised to use large tampons.
Surgical intervention to strengthen the anterior wall of the vagina.