One in ten people will experience a kidney stone at least once in their lifetime – and this statistic is increasing almost every year.
The risk of developing stones is multifactorial, depending on both internal factors (patient-specific – gender, age, family history, comorbidities) and external factors (fluid intake, diet, lifestyle, climate, country of residence).
However, the common belief that kidney stone disease is more prevalent in hot climates is not entirely accurate. For example, certain populations living in hot climates (e.g., Black Africans, Aboriginal Australians) have a low incidence of stones, whereas many regions with temperate climates (e.g., Northern Europe and Scandinavia) show a high incidence.
This may be linked to Western lifestyle patterns and the “epidemic” of obesity in Western societies – characterized by excessive food consumption, preservatives, inadequate fluid intake, limited physical activity, and poor dietary habits.
Obesity is associated with increased urinary excretion of stone-promoting substances – calcium, oxalate, uric acid – and decreased excretion of the stone-preventive substance citrate. Obese patients tend to have low urinary pH (high acidity), which promotes uric acid stone formation.
Men develop stones about three times more often than women, but the gender gap is narrowing. Testosterone may stimulate increased oxalate production in the liver (a precursor for calcium oxalate stones), while women tend to have higher urinary citrate levels (which inhibits calcium oxalate stone formation).
Nevertheless, as noted above, this gender difference is diminishing – likely due to metabolic disorders, inadequate hydration, sedentary lifestyles, and the widespread consumption of unhealthy foods.
About 25% of kidney stone patients report a family history of the condition. The relative risk remains high even after adjusting for dietary calcium intake.
Some inherited disorders predispose to stones, such as renal tubular acidosis (predisposing to calcium phosphate stones) and cystinuria (predisposing to cystine stones).
The use of extracorporeal shock wave lithotripsy (ESWL) for upper urinary tract stones increased by 55% between 2000 and 2010.
When kidney stones are diagnosed, a specific diet plan may be required. First, your physician will perform blood and urine tests to determine your individual risk factors. Based on these results, a tailored treatment and prevention strategy will be developed to help avoid future stone formation.
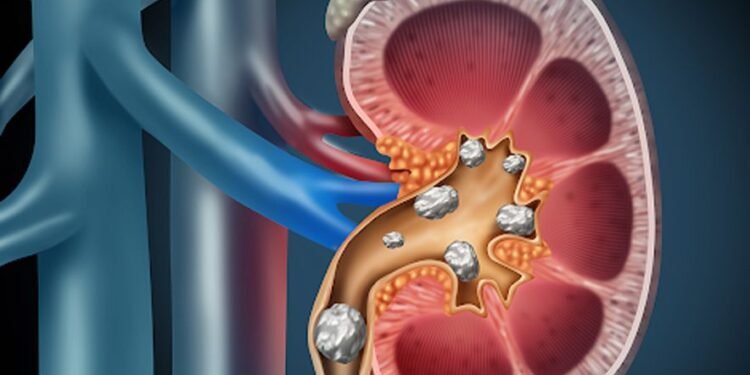
Kidney stones form from crystals present in the urine. For most people, natural urinary chemicals prevent stone formation.
Are all kidney stones the same?
No. The most common type is calcium-containing stones, followed by uric acid stones. Diet and medical treatment are chosen individually, depending on the stone type, to reduce the risk of recurrence.
What is the most important factor in preventing kidney stones?
One of the most effective measures is drinking plenty of water daily. Adequate hydration increases urination, which helps prevent the accumulation of calcium or uric acid crystals in the kidneys and urinary tract.
Don’t underestimate your sweat losses!
Activities such as sauna use, hot yoga, and intense exercise can be beneficial for health, but they may also trigger kidney stone formation. Why? Because sweating – whether from physical activity or hot weather – leads to fluid loss and reduced urination. Less urine means a higher concentration of minerals that can crystallize and form stones.
Drink plenty of fluids, especially during exercise or activities that cause heavy sweating. Aim for 2–3 liters (8–12 cups) of fluids daily to maintain optimal urine output, but consult your physician for your specific needs. Avoid sugary carbonated drinks (especially those high in fructose), sweetened iced tea, and grapefruit juice.
What kind of diet helps prevent kidney stones?
There is no single standard diet for kidney stone prevention. Dietary recommendations depend on the stone type and are tailored to each individual.
Calcium Oxalate Stones – The Most Common Type of Kidney Stones
Oxalate is a natural compound found in many foods, including fruits and vegetables, nuts and seeds, grains, legumes, as well as chocolate and tea. Some foods contain particularly high amounts of oxalate, such as peanuts, spinach, beets, chocolate, and sweet potatoes. Limiting these foods can be beneficial for people who form calcium oxalate stones.
Consume calcium-rich foods such as milk, yogurt, and certain cheeses – calcium binds with oxalate in the stomach and intestines, preventing it from reaching the kidneys and forming crystals. This is one effective way to reduce the formation of this type of stone in the urinary tract.
Calcium is not the enemy!
A common misconception is that calcium itself is the main cause of calcium oxalate stones. In reality, a low-calcium diet can actually increase the risk of kidney stone formation.
Do not reduce calcium in your diet. Instead, focus on reducing sodium intake and combining calcium-rich foods with oxalate-containing foods during the same meal. The recommended daily calcium intake for stone prevention is 1,000–1,200 mg.
Excess sodium increases the amount of calcium in the urine. Sodium and calcium are transported together in the kidneys, so eating high-sodium foods automatically increases urinary calcium excretion. This can raise the risk of calcium stone formation. Many foods contain “hidden sodium,” such as canned goods, processed foods, and fast food.
You can lower your sodium intake by choosing low-sodium foods. This will help reduce calcium in the urine and also aid in blood pressure control.
Uric Acid Stones – Another Common Type
Red meat, organ meats, and shellfish contain high amounts of purines, natural chemical compounds found in the body. A high purine intake increases uric acid production, raising the amount excreted by the kidneys. High uric acid concentration increases urinary acidity, facilitating uric acid stone formation.
To prevent uric acid stones, reduce intake of purine-rich foods such as red meat, organ meats, beer and alcoholic beverages, meat pies, sardines, anchovies, and shellfish. Follow a healthy diet primarily based on vegetables, fruits, whole grains, and low-fat dairy products. Limit sugary foods and drinks, especially those containing high-fructose corn syrup. Limit alcohol, as it can raise blood uric acid levels, and avoid short-term crash diets for the same reason. Reducing animal protein and increasing fruit and vegetable intake can help lower urinary acidity, potentially reducing uric acid stone risk.
Do Vitamin or Mineral Supplements Help or Harm?
B vitamins containing thiamine, riboflavin, niacin, B6, and B12 are not proven to be harmful for kidney stone formers. Some studies suggest vitamin B6 may help reduce high urinary oxalate levels. However, for supplements such as vitamin C, vitamin D, cod liver oil, or other calcium-containing minerals, it is best to consult your doctor or dietitian, as some may increase the risk of stone formation.
General Recommendations for Kidney Stone Prevention
-
Drink plenty of fluids: 2–3 liters of water daily, including other fluids such as water, coffee, and lemonade, which have been shown to be beneficial. Avoid grapefruit juice and soda.
-
Aim for a urine volume of at least 2.5 liters/day to keep urine dilute.
-
Limit high-oxalate foods, especially spinach, berries, chocolate, bran, nuts, beets, and tea.
-
Consume calcium-rich foods alongside other types of meals.
-
Avoid calcium supplements unless specifically prescribed by your doctor.
-
Consume moderate amounts of protein: Excess protein increases urinary calcium, raising stone risk.
-
Limit salt intake: High sodium raises urinary calcium and increases stone risk. Salt reduction is also important for blood pressure control.
-
Avoid high doses of vitamin C supplements: The recommended intake is 60 mg/day (U.S. Dietary Reference Intake). Excessive intake (1,000 mg/day or more) can lead to excess oxalate production in the body.